Subscribe to our periodic newsletter and get latest, relevant information on healthy living
There are many medical conditions that are influenced or induced by external factors and environmental cues. Some well-known examples are environmental-based allergies to such things as pollen, trees, grass, cat hair, termites, mold, and host of other ones. Food-based allergies or sensitivities, better known nowadays due to greater medical knowledge, improved diagnosis, and patient awareness, such as to common ingredients like eggs, milk, nuts, gluten, seafood among other specific allergens. Many health conditions, in fact majority of them, involve complex interplay between one’s genetic makeup and external factors or environmental inducers. Thus, it is relevant to examine and understand the role that overweight or obesity plays in the development of many other health conditions besides highly prevalent conditions that have been already presented herein. The role of being overweight or obese is important contributor to the various disorders presented below and a common theme emerges that emphasis the importance of weight loss through healthy living to significantly reduce or be free from being afflicted by such diseases. The varied type of diseases indicate the broad effects that being overweight or obese has in contributing to the causes of these disorders.
Cancer
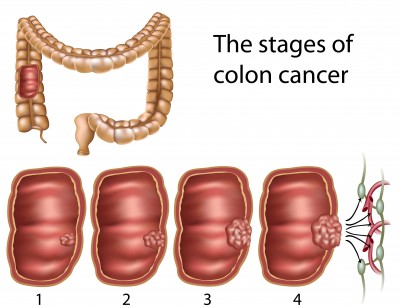
Cancer as a disease affects people of all ages, both genders, and different racial and ethnic background in varying degrees due to its multi-factorial etiology. It has been reported that worldwide deaths from cancer is ~7.9 million people according figures from year 2007; this number represents more than 13% of globally-reported deaths.1 Cancer is complex set of diseases caused by many intrinsic changes within cells and external risk factors that can affect nearly all tissues or any organ of the body. At the most basic level, cancer is disorder of uncontrolled cellular growth or proliferation and altered differentiation of cells in a given tissue where the growth of abnormal cells begin that if undetected can lead to formation of tumors therein and elsewhere in the body by process of metastasis into other tissues or organs of the body. It is the effects of uncontrolled tumor formation within the origin site of abnormal cell proliferation and other tissues or organ when routinely signs and symptoms of cancer are known to individuals or detected during medical testing. The use of many screening or routine medical tests for many forms of cancer like breast cancer in women, prostrate cancer in men, colon-rectal cancer, adenomatous polyps in gastro-intestinal tract, routine CBC’s with differentials (complete blood counts) for leukemia and lymphoma among others has allowed successful treatment and many times cure or remission from such cancers. Nonetheless, cancer is not completely preventable or curable yet like some other medical disorders such as certain infectious diseases, common metabolic disorders like lactose intolerance or alcohol sensitivity, vitamin or nutrient deficits, hormonal deficiency, food or environmental allergies and the like. The strides made in understanding this multi-factorial disease entity has allowed us to know about many risk factors that increase the chances of acquiring cancer in an individual’s life. The most common known risk factors are smoking for lung cancer, excessive and unprotected sun or UV (ultra-violet) exposure for types of skin cancer, excessive use of Betel nut or chewing tobacco with oral cancers, pre-menopausal use of high-dose of estrogen and certain forms of endometrial, ovarian and breast cancers,2 exposure to human papillomavirus (HPV strains 16,18) and cervical cancer are some well-known examples of cancers associated with such risks or external factors. Yet for many cancer types, the exact link between certain risk factors and onset of a particular cancer or abnormal tumor is known completely understood and remain subject to intense investigations and discoveries.
 Cancer or tumor formation of given cell type or tissue as mentioned above is uncontrolled and abnormal cellular proliferation and altered differentiation that arises when there are multiple changes or mutations in genes or DNA (the double-stranded helix of nucleic acids that is blueprint for all functions carried out within every cell of the body) of certain critical genes that control and govern timely cellular proliferation and growth. Interestingly, while genes can go awry or mutate or change within cells on their own, certain external factors highly increase the formation of abnormal and harmful mutations, these mutations can accumulate in normal cells up to critical point until sufficient number of mutations or genetic changes cause uncontrolled cell proliferation, if unchecked lead to formation of tumors, and subsequent manifestations of uncontrolled tumor growth within a given organ or part of the body to give rise to clinical disorder called cancer.
Cancer or tumor formation of given cell type or tissue as mentioned above is uncontrolled and abnormal cellular proliferation and altered differentiation that arises when there are multiple changes or mutations in genes or DNA (the double-stranded helix of nucleic acids that is blueprint for all functions carried out within every cell of the body) of certain critical genes that control and govern timely cellular proliferation and growth. Interestingly, while genes can go awry or mutate or change within cells on their own, certain external factors highly increase the formation of abnormal and harmful mutations, these mutations can accumulate in normal cells up to critical point until sufficient number of mutations or genetic changes cause uncontrolled cell proliferation, if unchecked lead to formation of tumors, and subsequent manifestations of uncontrolled tumor growth within a given organ or part of the body to give rise to clinical disorder called cancer.
One risk factor that increases certain types of cancer is obesity or excessive accumulation of adipose or fat tissue within the body. A published study revealed that over-all for all types of cancer, obesity (defined in study as being 40% more weight than average for given height) increased death from cancer by ~38% in men and by over 50% in women.3 Moreover, obesity predisposed men to die from certain forms of cancer such as colon, rectal, and prostrate cancer compared to non-obese men. In contrast, obese women had higher rates of breast, ovarian, endometrial, cervical and gallbladder cancer than healthy weight women.4 These findings are affirmed by other clinical studies that showed obese men are three times more likely to be afflicted with esophageal cancer than healthy weight men.5 For pre-menopausal women, carrying extra 10-18 lbs. of weight above their normal BMI increased the risk of developing breast cancer at later stages of their lives that is most likely due to having excess body fat and not dependent on intake of fats in their diets.6,7,8,9 It was found that carrying extra forty pounds of weight doubled the risk of breast cancer in post-menopausal women.9 While there is no guarantee that cancer will not arise in given individual due to the nature and manner in which this disease can arise, reducing external risks greatly diminishes the chances of many forms of cancer. In addition, studies have found out that being overweight or obese is substantial contributor to death from all forms of cancer. Indeed, obesity contributes to development of several types of cancer and accounts for 15-20% of cancer-related deaths.10,11 Conversely, cancer death attributed to suboptimal physical activity or the lack thereof which is highly associated with overweight and obese people is important risk giving rise to many types of cancer.10 Moreover, the role of diet and food choices plays a critical role in development of many types of cancer.12,13,14,15 Hence, if obesity is trigger that increases risk of certain forms of cancer in men and women, it serves the best interests of the individuals to embark on weight loss through healthy living to mitigate or even eliminate risk of cancer associated with being moderately overweight or obese.
Sleep Apnea
Sleep apnea is sleep disorder that is significant problem for adults and in some cases even children. However, it primarily affects adults and is characterized by episodes during sleep when there is stoppage of breathing or very low breathing rate. These episodes can be anywhere from few seconds to few minutes and occur many times during sleep up to 25-30 times per hour. The effects of this abnormal sleeping pattern is that people are sleep deprived, tired during day, have decreased daytime mental alertness, more prone to sleep during daytime, have decreased cognitive and memory functions, and more prone to emotional and behavioral problems stemming from lack of quality sleep.16 There are three major forms of sleep apnea, but the most common form which accounts for nearly 85% of sleep apnea is called obstructive sleep apnea (OSA). Obstructive sleep apnea occurs due to weaken muscle tone of the airway in region of throat, presence of soft tissue in this region, and certain mechanical features within their airways that causes greater collapse or obstruction of airway during breathing cycles of sleep. The most common factors that give to OSA in people are obesity, history of smoking, and age. As person ages with other predisposing condition like obesity, the risk of having OSA increases, too. Also, it is observed that sleep apnea affects men more than women or children. Additionally, people with diabetes or pre-diabetes are three times more likely to experience OSA. Other parameters that are seen in people with OSA is that they are obese with Body Mass Index (BMI>30), have above-average neck circumference (~17 inches in men and ~16 inches in women), have propensity to snore during sleep,17 have enlarged tonsils and tongues, are prone to daytime sleep, have problems with cognitive and memory functions, and as stated above can suffer from mood swings, depression and even sexual dysfunction. More importantly, people afflicted with OSA have greater risk for high blood pressure, stroke, cardiovascular disease, arrhythmias, diabetes, metabolic changes due to disturbed sleeping pattern, and prone to injury or accidents due to lack of quality nighttime sleep.18,19,20,21,22 The prescribed course to treat OSA has been to quit smoking for smokers, eliminating alcohol, and losing weight to reduce obesity that compromises their airways from functioning in normal manner during sleep. People suffering from sleep apnea, excessive snoring, and lack of good sleep can get relief. Hence, not only does overweight and obesity result in increased prevalence of many medical conditions, but it affects quality of life for something as natural and simple as nighttime sleeping. The importance of weight loss through healthy living can not be overstated since it benefits far outweigh the challenges to be expected in losing weight for the long-term.
Metabolic Syndrome
Metabolic syndrome is a recently described disorder that was first described in the medical literature in later part of 1950’s and become accepted part of medical usage in the 1970’s. It is estimated that ~25% of adult population has metabolic syndrome and it is highly associated with development of diabetes or impaired glucose intolerance and cardiovascular disease.23 It was estimated that 50% of patients with coronary heart disease had prevailing metabolic syndrome, while ~44% of adult population aged 50 and above were defined as having metabolic syndrome.24 Metabolic Syndrome also known as cardio-metabolic syndrome or metabolic syndrome X is health condition characterized by abnormal physiological parameters that increase the risks of developing diabetes and cardiovascular disease. According to U.S. National Cholesterol Education Program Adult Treatment Panel III (2001)25 people are defined with metabolic syndrome if at least three of the following criteria are met:
Central obesity: waist circumference ≥ 102 cm or 40 inches (male), ≥ 88 cm or 36 inches(female)
Fasting plasma glucose ≥ 6.1 mmol/L (110 mg/dl)
Dyslipidemia: HDL-C (high-density lipoprotein) < 40 mg/dL (male), < 50 mg/dL (female)
Dyslipidemia: TG (triglycerides or blood fatty acids) ≥ 1.7 mmol/L (150 mg/dl)
Blood pressure ≥ 130/85 mmHg
People who are diagnosed with metabolic syndrome have constellation of signs and symptoms marked by central or abdominal obesity, either frank diabetes or insulin resistance, hyperlipidemia (high blood fatty acids), subnormal or  low levels of HDL (high-density lipoprotein) or “good” cholesterol, high blood pressure and in many cases hyperuricemia and fatty liver or hepatic steatosis. The exact cause of metabolic syndrome remains unclear, but many risk factors greatly increase the onset of this disorder. The identifiable risk factors are obesity in particular central or abdominal obesity, older age, sedentary lifestyle (little or no physical activity along with excessive eating), and some form of insulin resistance. Most people with metabolic syndrome have deranged blood sugar levels despite large amount of secreted insulin or hyperinsulinemia (high insulin levels) and insulin can not carry out its normal function to regulate blood sugar levels. Another associated risk factor contributing to this disorder is stress; it is theorized based on clinical data that hypothalamic-pituitary-adrenal (HPA) axis is disrupted by stress.26,27 The abnormal functioning of HPA unit causes marked elevation of cortisol or stress hormone that in turn raises glucose and insulin levels. The higher levels of cortisol and insulin affect metabolism within fat cells or adipose tissue to increase their fat content, trigger insulin resistance, high triglycerides, and hypertension, too. The etiology or cause of metabolic syndrome has not been elucidated yet, but it appears to be due to complex interaction of factors. The primary factors are obesity, advanced age (>50 years old), genetics, sedentary lifestyle, stress, and some form of underlying endocrine disorder.28,29,30,31 Nonetheless, patients who are placed on low-calorie, healthy diet and with moderate form of exercise (like 30 minutes of daily walking) showed marked improvement on physiological parameters that define metabolic syndrome.32,33 Moreover, it was found that limiting amount of total carbohydrate rather than fat intake was more beneficial to diminish the common abnormal findings of metabolic syndrome.34 It is in the best interests of the overweight and obese that when afflicted with the signs and symptoms of metabolic syndrome that their medical condition should be promptly corrected by weight loss through healthy living.
low levels of HDL (high-density lipoprotein) or “good” cholesterol, high blood pressure and in many cases hyperuricemia and fatty liver or hepatic steatosis. The exact cause of metabolic syndrome remains unclear, but many risk factors greatly increase the onset of this disorder. The identifiable risk factors are obesity in particular central or abdominal obesity, older age, sedentary lifestyle (little or no physical activity along with excessive eating), and some form of insulin resistance. Most people with metabolic syndrome have deranged blood sugar levels despite large amount of secreted insulin or hyperinsulinemia (high insulin levels) and insulin can not carry out its normal function to regulate blood sugar levels. Another associated risk factor contributing to this disorder is stress; it is theorized based on clinical data that hypothalamic-pituitary-adrenal (HPA) axis is disrupted by stress.26,27 The abnormal functioning of HPA unit causes marked elevation of cortisol or stress hormone that in turn raises glucose and insulin levels. The higher levels of cortisol and insulin affect metabolism within fat cells or adipose tissue to increase their fat content, trigger insulin resistance, high triglycerides, and hypertension, too. The etiology or cause of metabolic syndrome has not been elucidated yet, but it appears to be due to complex interaction of factors. The primary factors are obesity, advanced age (>50 years old), genetics, sedentary lifestyle, stress, and some form of underlying endocrine disorder.28,29,30,31 Nonetheless, patients who are placed on low-calorie, healthy diet and with moderate form of exercise (like 30 minutes of daily walking) showed marked improvement on physiological parameters that define metabolic syndrome.32,33 Moreover, it was found that limiting amount of total carbohydrate rather than fat intake was more beneficial to diminish the common abnormal findings of metabolic syndrome.34 It is in the best interests of the overweight and obese that when afflicted with the signs and symptoms of metabolic syndrome that their medical condition should be promptly corrected by weight loss through healthy living.
References
1. Jemal A, Bray, F, Center, MM, Ferlay, J, Ward, E, Forman, D (February 2011). “Global cancer statistics”. CA: a cancer journal for clinicians 61 (2): 69–90.
2. Henderson BE, Bernstein L, Ross RK (2000). “Chapter 13:Hormones and the Etiology of Cancer.” In Bast RC, Kufe DW, Pollock RE, et al.. Holland-Frei Cancer Medicine (5th ed.). Hamilton, Ontario: B.C. Decker. ISBN 1-55009-113-1.
3. Lawrence Garfinkel, “Overweight and Cancer,” Annals of Internal Medicine 103 (6 pt. 2[December 1985]):1034-36.
4. F. Xavier Pi-Sunyer, “Health Implications of Obesity,” American Journal of Clinical Nutrition 53 (6[June 1991]): 1595S-1603S.
5. Linda Morris Brown et al., “Adenocarcimona of the Esophagus: Role of Obesity and Diet,” Journal of the National Cancer Institute 87 (2{18 January 1995]): 104-9.
6. “Weight Gain, Cancer Link Eyed,” Cancer Researcher Weekly, 30 May 1994, p.6.
7. “Weight Gain by Thirty May Raise Breast Cancer Risk,” St. Petersburg Times, 18 May 1994, p.4A.
8. Rachel Ballard-Barbash and Christine A. Swanson, “Body Weight: Estimation of Risk for Breast and Endometrial Cancers,” American Journal of Clinical Nutrition 63 (3 supp. [March 1996]): 437S-41S.
9. “Breast Cancer (Increased Risk): Increased Risk Associated with Weight, Not Fat Intake,” Cancer Weekly Plus [8 July 1996]:7.
10. Kushi LH, Byers T, Doyle C, Bandera EV, McCullough M, McTiernan A, Gansler T, Andrews KS, Thun MJ (2006). “American Cancer Society Guidelines on Nutrition and Physical Activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity,” CA Cancer J Clin 56 (5): 254–81; quiz 313–4.
11. Anand P, Kunnumakkara AB, Kunnumakara AB, Sundaram C, Harikumar KB, Tharakan ST, Lai OS, Sung B, Aggarwal BB (September 2008). “Cancer is a preventable disease that requires major lifestyle changes,” Pharm. Res. 25 (9): 2097–116.
12. Park S, Bae J, Nam BH, Yoo KY (2008). “Aetiology of Cancer in Asia,” (PDF). Asian Pac. J. Cancer Prev. 9 (3): 371–80.
13. Wicki A, Hagmann, J (September 2011). “Diet and cancer,” Swiss medical weekly 141: w13250.
14. Cappellani A, Di Vita M, Zanghi A, Cavallaro A, Piccolo G, Veroux M, Berretta M, Malaguarnera M, Canzonieri V, Lo Menzo E (2012). “Diet, obesity and breast cancer: an update,” Front Biosci (Schol Ed) 4: 90–108.
15. Key TJ (January 2011). “Fruit and vegetables and cancer risk,” Br. J. Cancer 104 (1): 6–11.
16. El-Ad, Baruch; Lavie, Peretz (2005). “Effect of Sleep Apnea on Cognition and Mood,” International Review of Psychiatry 17 (4): 577–582.
17. Morris LG, Kleinberger A, Lee KC, Liberatore LA, Burschtin O (November 2008). “Rapid risk stratification for obstructive sleep apnea, based on snoring severity and body mass index,” Otolaryngology–Head and Neck Surgery 139 (5): 615–8.
18. Yan-fang S, Yu-ping W (August 2009). “Sleep-disordered breathing: impact on functional outcome of ischemic stroke patients,” Sleep Medicine 10 (7): 717–9.
19. Bixler EO, Vgontzas AN, Lin HM, et al. (November 2008). “Blood pressure associated with sleep-disordered breathing in a population sample of children,” Hypertension 52 (5): 841–6.
20. Leung RS (2009). “Sleep-disordered breathing: autonomic mechanisms and arrhythmias,” Progress in Cardiovascular Diseases 51 (4): 324–38.
21. Silverberg DS, Iaina A, Oksenberg A (January 2002). “Treating Obstructive Sleep Apnea improves essential hypertension and life,” American Family Physician 65 (2): 229–36.
22. Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V (November 2005). “Obstructive sleep apnea as a risk factor for stroke and death,” The New England Journal of Medicine 353 (19): 2034–41.
23. Ford ES, Giles WH, Dietz WH (2002). “Prevalence of metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey,” JAMA 287 (3): 356–359.
24. Fauci, Anthony S. (2008). Harrison’s principles of internal medicine. McGraw-Hill Medical. ISBN 0-07-147692-X.
25. Expert Panel On Detection, Evaluation, And Treatment Of High Blood Cholesterol In Adults (May 2001). “Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III),” JAMA: the Journal of the American Medical Association 285 (19): 2486–97.
26. Gohill, BC; Rosenblum, LA; Coplan, JD; Kral, JG; (July 2001). “Hypothalamic-pituitary-adrenal axis function and the metabolic syndrome X of obesity,” CNS Spectr. 6 (7): 581–6, 589.
27. Brunner, EJ; Hemingway, H; Walker, BR; Page, M; Clarke, P; Juneja, M; Shipley, MJ; Kumari, M; Andrew, R; Seckl, JR; Papadopoulos, A; Checkley, S; Rumley, A; Lowe, GD; Stansfeld, SA; Marmot, MG; (November 2002). “Adrenocortical, autonomic, and inflammatory causes of the metabolic syndrome: nested case-control study,” Circulation. 106 (21): 2634–6.
28. Pollex, R.L.; Hegele, R.A. (2006). “Genetic determinants of the metabolic syndrome,” Nat Clin Pract Cardiovasc Med 3 (9): 482–9.
29. Poulsen, P.; Vaag, A.; Kyvik, K.; Beck-nielsen, H. (2001). “Genetic versus environmental aetiology of metabolic syndrome among male and female twins,” Diabetologia 44 (5): 537–543.
30. Groop, Leif (2000). “Genetics of the metabolic syndrome,” British Journal of Nutrition 83 (83): S39–S48.
31. Bouchard, G. (1995). “Genetics and the metabolic syndrome,” International journal of obesity 19: 52–59.
32. Lakka TA, Laaksonen DE (2007). “Physical activity in prevention and treatment of the metabolic syndrome,” Applied physiology, nutrition, and metabolism = Physiologie appliquée, nutrition et métabolisme 32 (1): 76–88.
33. Feldeisen SE, Tucker KL (2007). “Nutritional strategies in the prevention and treatment of metabolic syndrome,” Appl Physiol Nutr Metab 32 (1): 46–60.
34. Volek JS, Feinman RD (2005).”Carbohydrate restriction improves the features of Metabolic Syndrome. Metabolic Syndrome may be defined by the response to carbohydrate restriction,” Nutr Metab (Lond) 2 (1): 31.




I am impressed, I must say. Very seldom do I come across a blog that is both informative and entertaining, and let me tell you, you’ve hit the nail on the head. Your idea is important; the issue is something that not a lot of people are talking intelligently about. I am really happy that I stumbled across this in my search for something relating to it.